Keratoconus
What is keratoconus?
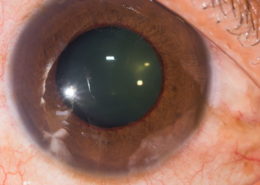
Keratoconus is an eye condition in which the normally round dome-shaped clear window of the eye (cornea) progressively thins causing a cone-shaped bulge to develop. Exactly why this happens is unknown, but genetic factors play a role and it is more common in people with allergic diseases such as asthma, in Down’s syndrome and in some disorders of connective tissue such as Marfan’s disease. It affects up to one in 1,000 people and is more common in people of Asian heritage. It is usually diagnosed in teenagers and young people.
How kerataconus affects vision
The change in shape and thinning of the cornea and, in later stages, scarring causing loss of transparency of the cornea impairs the ability of the eye to focus properly, causing poor vision.
Treatments for keratoconus
In the early stages, spectacles or soft contact lenses may be used to correct vision. As the cornea becomes thinner and steeper, rigid gas permeable (RGP) contact lenses are often required to correct vision more adequately. In very advanced cases, where contact lenses fail to improve vision, a corneal transplant may be needed.
Changes caused by keratoconus can take many years to develop. For this reason we monitor those with the condition and invite them back for repeat assessments. The following tests might be performed;
1. Vision (reading chart)
2. Refraction (spectacle test)
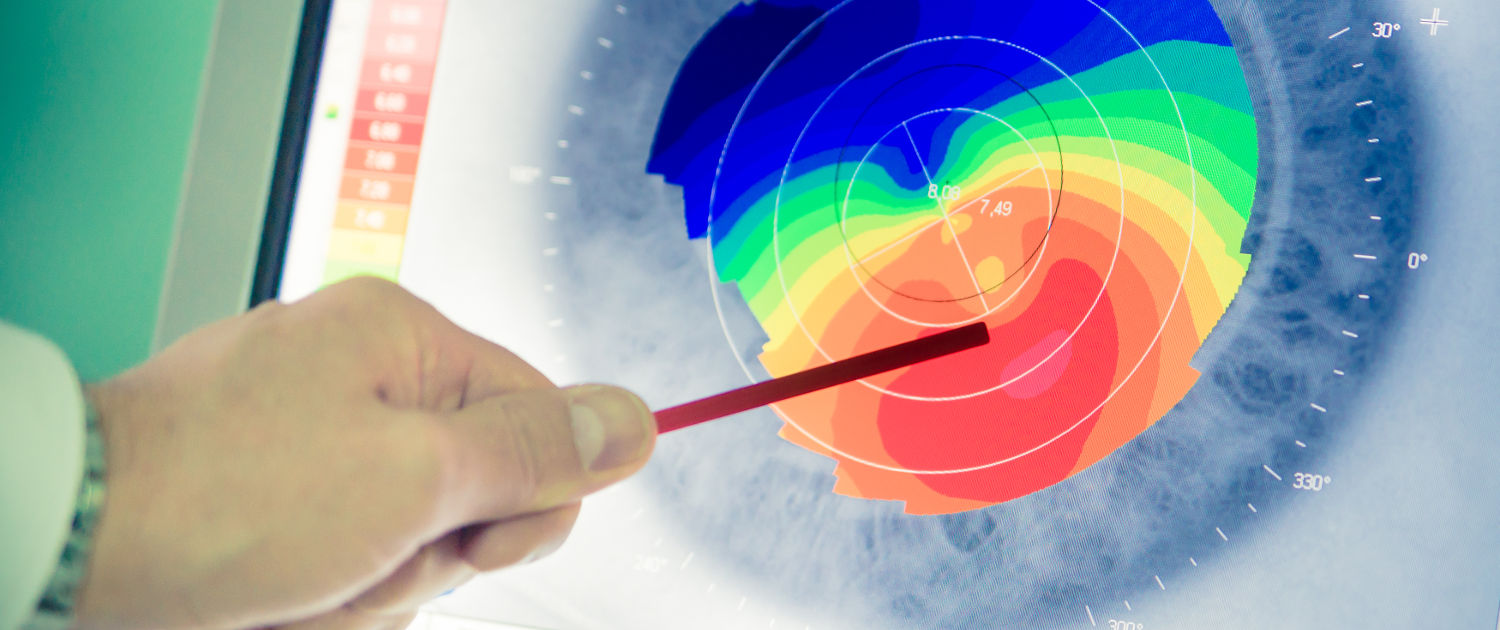
3. Corneal scan (Pentacam)
Any necessary contact lens checks will also be undertaken. The results are compared with those from your previous visits. If the results are getting steadily worse, we will discuss with you whether you need to undergo corneal cross-linking (CXL).
CXL is a new treatment that can stop keratoconus getting worse. It is effective in more than nine out of 10 patients, with a single 30-minute day-case procedure, but it is only suitable where the corneal shape is continuing to deteriorate. Beyond a certain stage, if the cornea is too thin, it could be unsafe to perform the procedure. Usually in people in their late 30s, the cornea naturally stiffens and CXL is generally not required. Below this age, the cornea is more flexible and disease progression (and worsening vision) are more likely to occur.
Discover the other pathologies
This post is also available in: Italian