Diabetic retinopathy
What Is Diabetic Retinopathy?
Diabetes is a condition in which the human body’s ability to transform and store sugar is impaired. Among the characteristics of the disease there are gradual transformations of the blood vessels. Diabetic retinopathy is a complication of diabetes caused by the deterioration of the vascular system that nourishes the retina in the back of the eye. Because the blood vessels weaken, they may lose fluid or blood in the transparent vitreous mass that fills the eye, or they may dilate, damaging the retina, a very delicate structure.
Who is at risk?
Many diabetics, especially those with poor control of diabetes leading to too high levels of blood sugar for long periods of time, have damaged retinal blood vessels. People who have had diabetes for many years are particularly at risk of developing diabetic retinopathy. Eight people in ten of those who have had diabetes for over ten years show symptoms of retinal damage; high blood pressure and pregnancy worsen the situation.
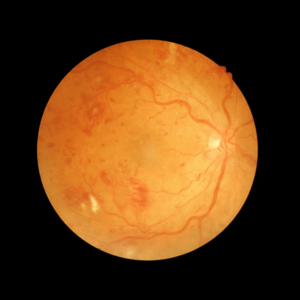
Exudative retinopathy
In exudative retinopathy, blood vessels weaken and begin to lose blood and serum. These fluids accumulate and form deposits in the retinal tissues, making them edemize. If the blood vessels are in the peripheral area of the retina, there is usually no serious weakening of the sight. If the fluid accumulates in the macula – the part of the retina responsible for the distinct vision, details and colors – dark spots and darkened vision can make it difficult or impossible to read or to drive.
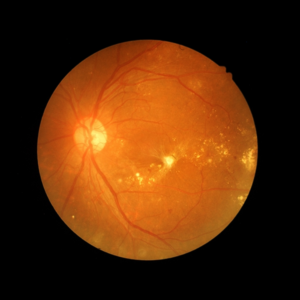
Proliferative retinopathy
In the second and most advanced stage of diabetic retinopathy, abnormal vessels spread – proliferate – through the inner surface of the retina. These weakened vessels can bleed into the vitreous and prevent light from reaching the retina. In addition, the wounded connective tissue, which is formed as a result, can contract by pulling the retina away from the underlying structure and causing it to detach itself. As a result of this, a severe loss of sight can occur, and blindness can also occur.
Symptoms
There is no pain in both forms of retinopathy.
There may be a gradual blurred vision, but without a medical examination some changes in the eye may not be detected. In proliferative retinopathy, when there is bleeding, the patient may see stains, blurred vision, or experience a complete loss of sight in the affected eye.
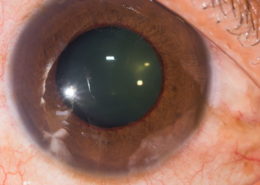
Exams and diagnosis
Regular eye visits are essential for all diabetics, so signs of diabetic retinopathy can be identified as soon as possible. If a person is diabetic and has a visual blur, he/she should contact an ophthalmologist. The ophthalmologist uses numerous tools and techniques to examine the retina. The slit lamp is used together with a lens to see the parts of the retina in the smallest details. The ophthalmoscope is frequently used to examine both the central and retinal part of the retina. In both cases, the pupil has to be dilated to examine the retina. In some cases, it is necessary to perform an exame called fluorangiography. The dye that is injected takes only a few seconds to reach the retina and make small blood vessels visible. These are then photographed to be thoroughly examined. Fluorangiography helps us to understand whether it is necessary to do laser.
Treatment
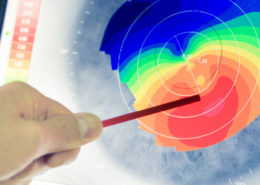
Consider the age of the patient, his clinical history, his lifestyle, and the degree of damage he has suffered from the retina before recommending an action line. In many cases treatment is not required, in others laser treatment may be advisable to stop the further progression of the disease. In the case of an exudative retinopathy, the laser heat seals the vessels and helps to hold the retina at the back of the eye forming small scars, thus reducing the fluid diffusion from the vessels. Other available treatments that show benefit to patients with diabetic macular edema are anti-vegf (anti-angiogenetic) drugs that are injected into the vitreous. A widespread treatment for proliferative retinopathy is called panretinic photocoagulation. In this process, the peripheral portion of the retina is scattered with laser light beams. Although a certain amount of healthy tissue is destroyed, this technique generally stops the further growth of abnormal cells and preserves the macula, saving a precious part of vision.
Vitreous removal
If the vitreous bleeds alone, a surgical procedure called vitrectomy may be recommended. In this technique the vitreous is aspirated and replaced with a transparent artificial solution.
Retinal detachment
Retinal detachment occurs when the transparent retinal layer separates from the pigmented layer. Since the cones and rods contained in the transparent layer are raised, the vision becomes obscured and distorted. Full detachment leads to loss of sight. Surgery to re-attach the retina is done in general or local anesthesia. First, the retinal ruptures are localized and welded using cryotherapy; then the vitreous fluid is drained from behind the transparent layer of the retina; Finally a silicone band is wrapped around the eye to indent and push the transparent and pigmented status again in contact with each other. The scar tissue that forms in the frozen areas re-attaches the retinal layers.
Conclusion
Those with diabetes may be affected by diabetic retinopathy. Examination and timely diagnosis are important to maintain a good vision. Since there are no symptoms at the initial stages, regular checks by an eye specialist are very important.
Discover the other pathologies
This post is also available in: Italian